Breast and ovarian cancers are two of the most prevalent and dangerous tumors that women get around the world. Over the years, scientific research has shown that the breasts and ovaries are biologically related, even though they are in distinct areas of the body. Genetics play a crucial role in this association, especially when the BRCA1 and BRCA2 genes change. It’s crucial to know how these mutations change the way cancer grows and to find common risk factors and techniques to stop it from growing so that cancer can be found early and treated successfully.
BRCA1 and BRCA2 are two genes that stop tumors from growing. They usually mend broken DNA, which maintains the cell’s genetic material stable. But when these genes are changed, they can’t safeguard cells, which could make them grow too quickly and maybe even cause cancer. Women who have a harmful alteration in either BRCA1 or BRCA2 are far more likely to have breast or ovarian cancer. Both parents can make these changes, not just moms. This means that both men and women can carry these mutations and pass them on, even if they never get cancer. This argument shows how vital it is to know the medical history of both sides of the family.
The American Cancer Society and a lot of other studies say that women with a BRCA1 mutation had a 72% chance of having breast cancer and a 44% chance of getting ovarian cancer in their lifetime. Women with a BRCA2 mutation are less likely to get breast cancer (up to 69%) and ovarian cancer (up to 17%), but the risks are still substantial. You have a 1.3% probability of having ovarian cancer in your lifetime and a 13% chance of getting breast cancer. These numbers show that there has been a huge rise compared to the average person.
These tumors help each other in a good way. A woman is more likely to have ovarian cancer if she already has breast cancer, especially if she was diagnosed with it when she was young or if her family has a lengthy history of the disease. People who had breast cancer were about twice as likely to get ovarian cancer as people who didn’t have breast cancer, according to research. People with BRCA mutations are more likely to have this link, although people without detectable mutations may also be at higher risk because of common lifestyle, hormonal, or environmental variables.
Your family history is still one of the best methods to tell if you might get sick. If a woman’s mother, sister, or daughter has had breast or ovarian cancer, she is far more likely to get it herself. This is especially true if a lot of female relatives got one or both types of cancer when they were younger. Getting genetic counseling and BRCA testing can save lives for families. A positive test doesn’t imply a woman will develop cancer, but it could give doctors important information that helps them keep a closer eye on her and do things to avoid her from getting it.
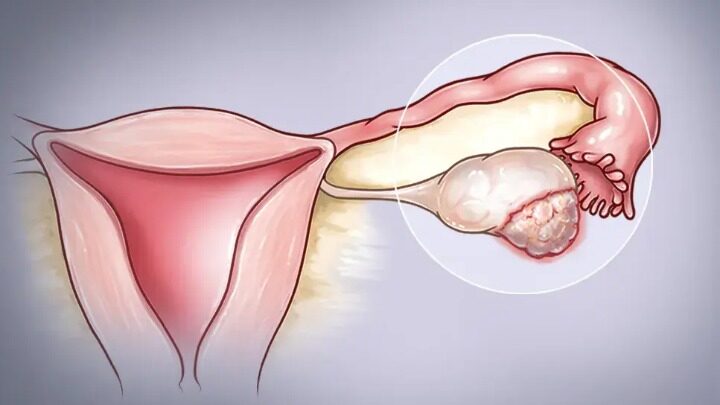
You have more choices for avoiding it before it starts or finding out about it early if you know how often it is to happen in your family. One method to do this is to have more screenings. Women who are at high risk for breast cancer may start getting screenings earlier than most women. They sometimes use both mammograms and breast MRIs together to acquire better findings. It’s still challenging to discover ovarian cancer early, but certain women who are at high risk may have blood tests and transvaginal ultrasounds on a regular basis to screen for symptoms of the disease.
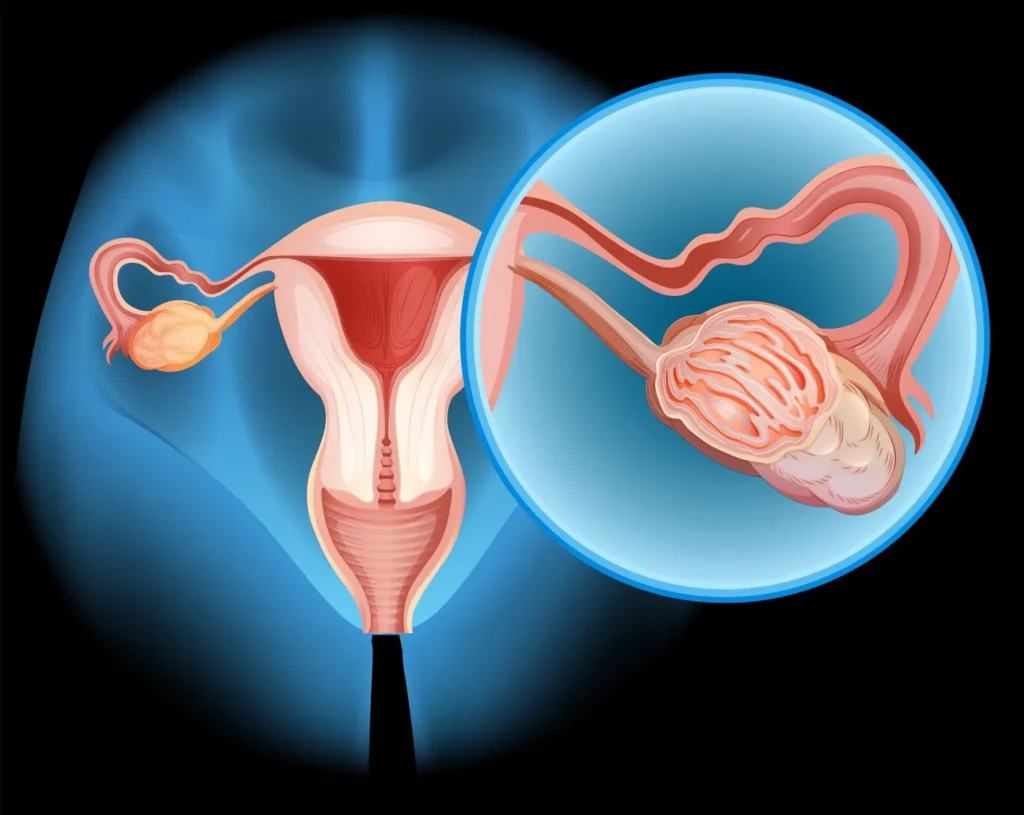
In more serious cases, people who are at high risk may decide to have surgery to lower their risk. People with the BRCA mutation can minimize their risk of breast cancer by up to 95% by having a preventive mastectomy, which involves the removal of one or both breasts. Removing the ovaries and fallopian tubes as a preventative measure could cut the incidence of ovarian cancer by up to 90%. Before menopause, lowering hormone levels may also dramatically lower the risk of getting breast cancer. These are big surgeries that affect both the psyche and the body, but many women think the trouble is worth it because it could lower their risk of getting cancer by a lot.
There are additional choices that have to do with drugs. Selective estrogen receptor modulators (SERMs), such as tamoxifen and raloxifene, can lessen the risk of breast cancer in women who are at high risk by blocking the effects of estrogen. Estrogen can make some breast tumors grow. These drugs are less invasive than surgery, but they do have adverse effects and aren’t suited for everyone.
Genetics aren’t the only thing that can make you more likely to have breast or ovarian cancer. Other aspects are also significant, like how you live and how you have kids. As you get older, each of these things are far more likely to happen. Obesity is another significant risk factor since having too much body fat can raise estrogen levels, which can then feed tumors that are sensitive to hormones. Women who have never been pregnant or who have never finished a pregnancy may also be at higher risk. This could be because their ovulatory cycles are still going on, which means they have more hormones in their bodies. Hormone replacement therapy (HRT), especially estrogen-progestin therapy, has also been associated to a higher risk of both types of cancer when administered for a long time after menopause.
It’s alarming to consider that your genes might make you more likely to have cancer, but the good news is that knowing this gives you power. Women may now be able to take better care of their health than ever before since they know more, can receive genetic testing faster, and can get medical care that is made just for them. Women who are more likely to get sick should talk to their doctors about how to keep healthy. To stop the problem, you may need to adjust your lifestyle, take medicine, get checked more often and earlier, or even have surgery.
In conclusion, there is a strong and clear link between ovarian and breast cancer, even though they happen in distinct parts of the body. This is very essential because the BRCA1 and BRCA2 genes have changed. This knowledge can help women figure out how likely they are to have cancer, make informed choices, and do things to avoid getting it or identify it when it’s easiest to treat. To stop these deadly diseases, you need to identify them early, know your family’s health history, and have access to the newest tests and treatments.
